What is Diabetic Retinopathy
Diabetic retinopathy is an eye problem that can be caused by either type 1 or type 2 diabetes mellitus. Retinopathy occurs when diabetes damages the tiny blood vessels in the retina. The weakened blood vessels may leak fluid and blood.
Diabetic Retinopathy is caused by Diabetes Mellitus which is a multisystem disorder affecting the heart, kidneys, peripheral nerves and eyes. Involvement of the retina is called diabetic retinopathy, and can lead to blindness. In chronic diabetic patients (duration of more than twenty years), nearly all patients with type I diabetes (insulin-dependent) and more than 60% of those with type II diabetes (non-insulin dependent) will have some degree of retinopathy. This also depends on how well the disease has been controlled.
There are two forms of diabetic retinopathy: non-proliferative (NPDR) and proliferative (PDR). Non-proliferative diabetic retinopathy refers to the early stages of the disease, while proliferative diabetic retinopathy refers to the severe, progressive stage.
Macular edema: The fluid and exudates collect in the macula, the central part of the retina that helps us in fine central vision.

Risk for developing diabetic retinopathy – Those with poorly controlled blood sugar levels are at a high risk of developing diabetic retinopathy. In addition, high blood pressure, high cholesterol, anemia, kidney disease and pregnancy can all place a patient at greater risk of suffering from diabetic eye disease.
Symptoms
There may be no symptoms in the early stages, especially when the central portion of the retina is not involved. As the retinopathy progresses, you may have:
- Blurred vision
- Floaters, which can look like black spots, little threads, or cobwebs
- Bleeding in the eye causing sudden loss of vision
- Temporary or permanent loss of vision.
Pain is not a common feature of the disease.
What your doctor looks for:
Your doctor would like to know
- Any family history of diabetes
- Any other systemic disease like hypertension or other lifestyle related disease and
- Any chronic use of cortico steroids
Diagnosis of diabetic retinopathy
a. Fundus Examination
b. Fundus Fluorescein Angiography
This diagnostic procedure utilizes a specialized fundus camera or scanning laser ophthalmoscope to capture rapid-sequence photographs of the retina following an intravenous injection of fluorescein sodium. Photographic or video images taken as the dye courses through the eye can demonstrate abnormalities within the neurosensory retina, pigment epithelium, sclera, choroid, and optic nerve, providing clinically useful information for nearly the entire spectrum of posterior segment disorders.
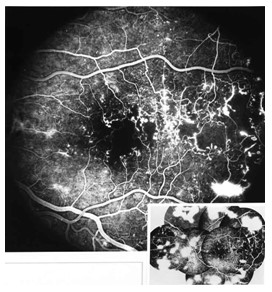
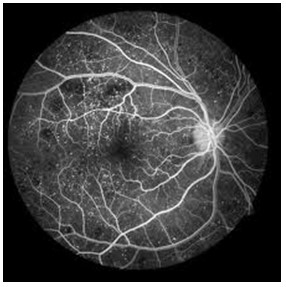
DR 1 DR 2
c. Optical Coherence Tomography
Optical coherence tomography (OCT) is a non-invasive imaging test that uses light waves to take cross-section pictures of your retina, the light-sensitive tissue lining the back of the eye.
With OCT, each of the retina’s distinctive layers can be seen, allowing mapping and measurement of their thickness. These measurements help with diagnosis and provide treatment guidance for glaucoma and retinal diseases, such as age-related macular degeneration and diabetic eye disease.
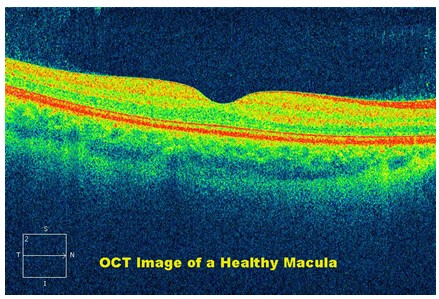

Macular Oedema in Diabetic Retinopathy
Prevention
The only way to prevent the development of diabetic retinopathy is strict control of blood sugar levels and regular exercise.
Treatment of Diabetic Retinopathy
a. Frequency of eye examination
If you have diabetes, you should get a yearly examination by your doctor. Once you develop diabetic retinopathy, your ophthalmologist may advise further investigations or treatment. A periodic follow up as advised by your ophthalmologist is mandatory. The frequency of these follow up visits is decided based on the severity of the disease.
b. Laser treatment
The aim of this treatment is to protect central vision. It does not restore lost vision, but it can prevent further deterioration, which is why early diabetic retinopathy diagnosis through periodic eye examination is imperative.
Laser photocoagulation involves tiny burns to seal the capillaries. This may cause small spots to appear in your field of vision after the procedure. These spots generally fade and disappear with time. Some patients may experience difficulties in dim illumination and while reading following multiple sittings of laser treatment.
c. Anti VEGF agents: In form of intravitreal injection
Anti VEGF agents are another modality of treatment for various stages of diabetic retinopathy. These agents are injected into the eye (intravitreal injection). They are commonly used in diabetic maculopathy and proliferative diabetic retinopathy. They may also be used as an adjunct before surgery for diabetic vitreous hemorrhage.
b. Vitrectomy
Vitrectomy is a surgical procedure in which cloudy, blood filled vitreous and scar tissue causing tractional retinal detachments are removed from the eye.
Know more:
Age Related Macular Degeneration (AMD)
CONTACT US
Address: Pakhowal Road, Opp. HDFC Bank, Jodhan, Jodhan Road, Ludhiana, Punjab (142029)
Mobile: +91-95690-67310
Email: info@digitaldoctors.ca
Web: https://grewaleyecare.com
